The Sunshine Act is sending ripples across the MedComms profession, both in the US, where it applies, and elsewhere. While the medical profession and pharmaceutical clients assess their responsibilities and develop their own responses to the legislation, here’s a very brief summary of the new requirements:
- Enacted to enforce public disclosure of financial relationships between the pharmaceutical industry and medical professionals
- Requires annual reporting of payments, or ‘transfers of value’ provided to physicians or teaching hospitals (first reporting date March 2014; ‘Transfer of value’ includes medical communications services)
- Applicable to any company that operates or markets a compound within the US, and to any interactions with US medical professionals regardless of location
(adapted from ISMPP Sunshine Act Task Force)
Undoubtedly, addressing perceived or actual conflicts of interest within medicine is timely and appropriate. In complex environments, however, it’s not until such policies have been road-tested that all of their consequences start to become apparent.
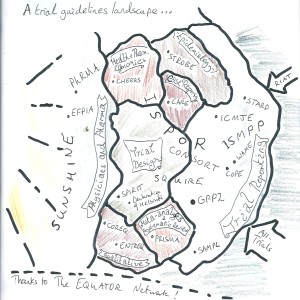
At the 6th Publication Plan meeting in London, supported by Adis Journals and organised through MedComms Networking, these consequences were explored by a roomful of medical publications professionals. Liz Wager (Publications Consultant, Sideview) gave an excellent and comprehensive presentation of the guidance and legislation concerned, both old and new.
One main point of discussion was exactly how MedComms services are interpreted as ‘transfer of value’ (TOV) under the Sunshine Act. In general, if medical professionals are required to declare medical writing, editing or analytical assistance personally as TOV, it could have a real impact on their willingness to accept such assistance. This could in turn reduce the number and quality of publications they are prepared to author, as the perception of such payments will be less positive than, for example, research funding. ISMPP state that ‘payments for medical research writing and/or publication would be included in the research payment, if the activity was included in the written agreement or research protocol’, but this is not always done, and it can be challenging to estimate the amount required accurately. The worst-case outcome could be fewer papers and less thorough reporting of studies, contradicting the drive for greater transparency.
An recent update from ISMPP suggests two interpretations of TOV in relation to assistance with medical publications. One proposal is to divide the TOV equally between authors (such that having more authors would minimise the impact on each author’s balance sheet!). However, dividing TOV equally between authors could be contentious given differences in contribution, and international authors would be exempt. There’s a further grey area concerning the TOV represented by specific services, for instance, a primary publication. Industry averages exist, but there’s no list of ‘fair market values’ as proposed by ISMPP as an alternative option. Whether this will turn out to be workable is not yet clear.
As other nations begin to draft and adopt similar legislation, as has already occurred in France, it will pose a challenge to the pharmaceutical industry to ensure that all regulatory requirements are met. Get in touch with Peter Llewellyn and the MedComms Network to get involved in the discussion and communicate with others involved in medical publications.